Can I Keep My Cat If I’m Pregnant?
Toxoplasmosis
When you decide it’s time to start a family, or when you have had the exciting news of a pregnancy, thoughts turn to the arrival of a healthy baby. If you’re a cat owner, perhaps you may have heard of toxoplasmosis and its potential to have serious consequences for your baby. Firstly, rest assured that you don’t have to get rid of your cat – you can safely manage the risks.
What is toxoplasmosis?
Toxoplasmosis is an infectious disease caused by a protozoal parasite known as Toxoplasma gondii and can affect many animals, including humans, mammals (including farm animals and cats), rodents and birds. It is prevalent world-wide.

How are cats involved in the life-cycle of toxoplasmosis?
Cats are the definitive host for Toxoplasma gondii and can acquire toxoplasmosis by hunting and eating infected animals, such as rodents and birds (intermediate hosts), or less commonly through ingestion of infected cat faeces. Oocysts excreted in cat faeces sporulate and the sporulated oocysts become infective approximately 24-48 hours later. This means that the cat itself is not a source of oocysts, only its faeces are.
Generally, cats only excrete the oocysts for 2 weeks after their initial infection. If the conditions are right (moist soil or water) these can remain viable in the environment for over 12 months! Cats are the only host that can support the entire life cycle of the parasite. This is known as the enteroepithelial life cycle.
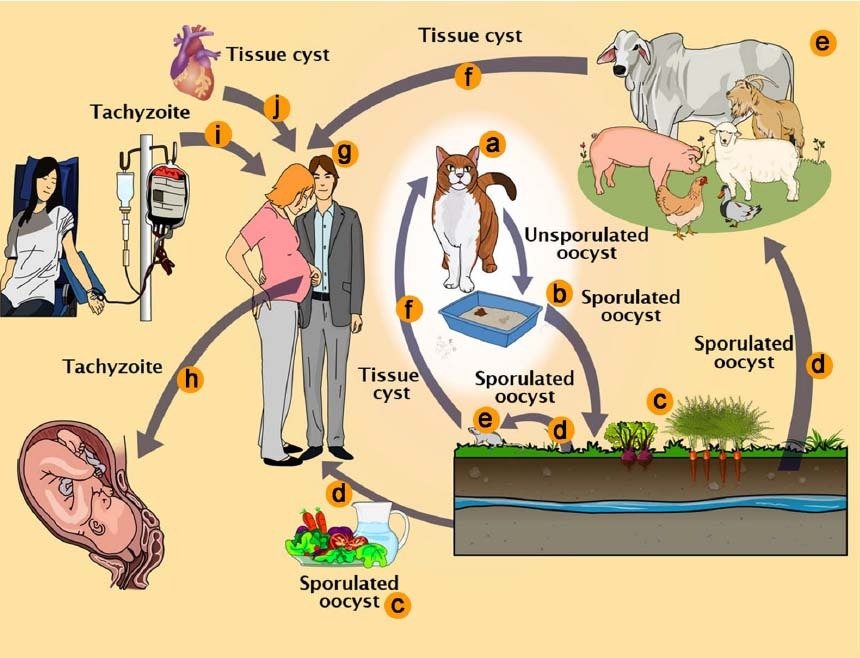
Toxoplasma gondii pathways of transmission. a Feline definitive host (cat). b Unsporulated oocysts in cat faeces. c Food contaminated with sporulated oocysts. d Oocysts may be ingested by intermediate hosts via water or raw vegetables. e Intermediate hosts (e.g. cattle, sheep, poultry and swine). f Ingestion of tissue cysts in uncooked meat. g Intermediate hosts (humans). h Tachyzoites transmitted through the placenta to the foetus. i Transmission by blood transfusion and organ transplant (j)
Diagram courtesy of and copyright of The life‑cycle of Toxoplasma gondii reviewed using animations
What are the clinical signs of toxoplasmosis in an infected cat?
Not all cats develop clinical disease and can be asymptomatic even while shedding infective oocysts in the faeces (particularly adult cats with well-developed immune systems).
Clinical disease caused by toxoplasmosis can be systemic or focal and reflect specific organ involvement.
Clinical signs of feline toxoplasmosis include:
- Diarrhoea
- Fever
- Lethargy
- Not eating
- Difficulty breathing (lung disease)
- Jaundice (liver disease)
- Neurological signs (CNS disease)
- Blindness or ocular lesions (eye disease)
Due to their immature immune system, kittens are more likely to develop clinical signs from toxoplasmosis compared with older cats. Breeds such as the Birman, Norwegian Forest and Persian cats are more susceptible to infection. Other risk factors for cats to develop severe disease include cats that have Feline Immunodeficiency Virus (FIV), Feline Leukaemia Virus (FeLV) or Feline Infectious Peritonitis (FIP) or those that are on immunosuppressive medication such as cyclosporin.
Clindamycin antibiotics is the treatment of choice in cats.
How can I prevent my cat from contracting toxoplasmosis?
Keeping your cat indoors will reduce the chance of your cat contracting Toxoplasma gondii, as hunting and scavenging are the main sources of infection.
Additionally, it is sensible to avoid feeding raw or undercooked meat to your cat, to avoid ingestion of infective tissue cysts. If your cat is on a special diet involving meat, then always freeze the meat for a minimum of 3 days to kill any tissue cysts first, though this is not considered a reliable method to prevent transmission and it is preferable to cook it thoroughly.
Another possible source of infection is via vectors such as cockroaches, so monitor your home environment closely.
Can dogs get toxoplasmosis?
Toxoplasmosis is an uncommon primary disease in dogs and mostly affects juvenile dogs. Unlike cats, you cannot catch toxoplasmosis through dog faeces, but dogs that eat cat faeces can shed oocysts for 2 days afterwards.
The most common clinical signs of canine toxoplasmosis are:
- Hind limb stiffness or paralysis
- Muscle pain
- Neurological signs such as tremors, seizures or focal loss of nerve function
- Blindness or ocular lesions
- Vomiting and diarrhoea
- Coughing and breathing difficulties
Clindamycin antibiotics is the treatment of choice in dogs.
What are the clinical signs of toxoplasmosis in an infected person?
Toxoplasmosis is extremely common and in fact, 80% of humans that contract toxoplasmosis are asymptomatic, so do not know that they have been infected.
For those that develop symptoms, the disease can range from a mild cold or flu-like illness to symptoms that mimic glandular fever and last for 1-12 weeks. The most common signs in humans are:
- Enlarged lymph nodes
- Muscle pain
- Joint pain
- Fever
- Lethargy
Toxoplasmosis infection persists for life, lying dormant in the body if an individual’s immune system is functioning well. For most healthy adults, toxoplasmosis doesn’t post any problems. Dormant infection can be reactivated in an immunosuppressed person, such as somebody on chemotherapy or in HIV-positive people. The most common signs in immunosuppressed people are:
- Inco-ordination
- Seizures
- Difficulty breathing
- Blurred vision
- Confusion
How do people contract toxoplasmosis?
The most common way that people become infected is by eating raw or undercooked meat (especially lamb, pork, kangaroo or venison), poultry or seafood infected or contaminated with Toxoplasma gondii cysts. Animals can harbour infective Toxoplasma gondii cysts in their tissues, especially in their brain and muscles, which can remain viable for extended periods. Other sources of infection include contaminated unpasteurised milk, contaminated unfiltered water or contaminated unwashed fruit and vegetables.
Another source of infection is through accidental ingestion of infective oocysts from cat faeces after cleaning out the litter tray or when gardening, by touching your mouth afterwards. To avoid this, wear gloves during gardening and always wash hands thoroughly after cleaning out your cat’s litter tray.
Children can become infected by ingestion of oocysts while playing in contaminated dirt or sandpits where an acutely infected cat has toileted. Only cats that are in an active stage of infection can shed the infective oocysts in their faeces. After this, the organism lies dormant in the cat’s body tissues and is no longer shed in the faeces. The cat itself is not considered a direct source of infection as faecal exposure is necessary for transmission to people.
Simply putting a contaminated hand or finger into your mouth could result in infection.
Less commonly, toxoplasmosis can be transmitted through blood transfusion or organ transplantation.
Toxoplasmosis cannot be transmitted directly from one person to another, except via the placenta during pregnancy, which is why pregnant women need to take extra precaution against infection.
How does Toxoplasma gondii affect an unborn child?
While toxoplasmosis acquired after birth usually results in either asymptomatic infection or mild illness, acute toxoplasmosis acquired in pregnancy can seriously affect the unborn child. If infected for the first time during the early stages of pregnancy (primary infection), toxoplasmosis can affect the baby’s brain, liver, spleen and eye development, whereas infection in the later stages of pregnancy can result in recurrent eye infections. In some cases, infection can result in miscarriage or stillbirth.
Sometimes babies with toxoplasmosis do not have any signs of infection and it is discovered later during schooling years, when symptoms such as hearing loss, severe eye infections and mental disability are identified.
Approximately 75% of women of child-bearing age are susceptible to primary infection with toxoplasmosis. While primary infection during pregnancy is rare, approximately 30% of these cases result in transplacental spread to the developing foetus, so prevention is better than cure.
Many women have already been exposed to toxoplasmosis prior to falling pregnant. The biggest risk is when a previously unexposed pregnant women contracts toxoplasmosis for the first time, as they have no immunity to it.
How is toxoplasmosis diagnosed in humans?
Toxoplasmosis is usually diagnosed with a blood test called serology, which looks at the levels and types of antibodies directed against Toxoplasma gondii. Usually the Toxoplasma-specific IgG antibodies are present 2-3 weeks after acute infection and then peak within 6-8 weeks.
If there are no Toxoplasma-specific IgG or IgM antibodies present, then this indicates that a person has likely not had previous exposure to the parasite.
By looking at the levels Toxoplasma-specific antibodies, a doctor can determine if an infection is active or dormant.
Other ways to obtain a positive diagnosis of toxoplasmosis include biopsy or PCR testing. In pregnancy, if there is a concern about an unborn baby contracting toxoplasmosis, a PCR test on amniotic fluid as well as an ultrasound may be recommended.
Should I test my cat for toxoplasmosis if I am pregnant?
Testing healthy cats for the presence of Toxoplasma gondii is not recommended because cats that test negative for toxoplasmosis (seronegative) actually present a higher risk to owners than those that test positive (seropositive). This is because the primary infection is when the cats excrete the infective oocysts.
Seropositive cats are generally immune to recurrent primary infection for around 6 years, then this can wane, which means that regardless of whether your cat is negative or positive, the same precautions are required.
How can I avoid toxoplasmosis if I am pregnant?
Pregnant women are advised to take the following precautions to avoid toxoplasmosis:
- Cook meat thoroughly (well-done)
- Avoid undercooked cured meat
- Avoid sashimi (raw seafood and fish)
- Do not consume unpasteurised milk or unpasteurised dairy products
- Wear gloves when preparing meals with raw meat and thoroughly wash hands afterwards
- Do not reuse utensils and cutting boards that have been used for raw meat preparation without thoroughly cleaning first in hot water and detergent or putting through a hot dishwasher cycle
- Do not eat or taste meat before it is finished cooking
- Avoid using the microwave to cook meat as microwaves do not heat evenly enough to reliably kill the organism
- Wash hands thoroughly before eating
- Avoid exposure to uncovered sandpits
- Wear gloves when handling soil or gardening and wash hands thoroughly afterwards
- Delegate cleaning cat litter trays to another family member where possible or wear gloves and wash hands thoroughly afterwards
- Always empty cat litter trays immediately after a cat defecates then wash tray with hot water to prevent oocysts becoming infective (which takes 24-48 hours after defecation)
- Dispose of cat litter tray contents properly and not into the garden and remember to clean the litter scoop too
- Prevent any dogs in the household from gaining access to cat toileting areas
- Feed your cat commercial cat food only and do not allow them to eat raw meat or hunt, especially while you are pregnant
Can I keep my cat if I’m pregnant?
Absolutely! Cats are great company while on maternity leave, or in the middle of the night while tending to your baby and if you take the simple precautions recommended above, there is no need to rehome your cat during pregnancy or after the baby is born.
Where can you obtain medical advice regarding toxoplasmosis?
It is important to consult with your GP, obstetrician or medical professional if you are concerned about toxoplasmosis or develop any clinical signs of concern during pregnancy.
Further resources for toxoplasmosis
Below are some further resources that you or your vet can access to assist with understanding toxoplasmosis.
Australian government toxoplasmosis pregnancy care guidelines
Victorian government toxoplasmosis pregnancy care guidelines
Information on toxoplasmosis in humans including babies, children and adults
Veterinary partner website article for non-veterinarians entitled: Toxoplasmosis in Cats
Veterinary scientific article entitled: Feline Toxoplasmosis


